[2006] An Introduction to The Integrated Systems Model in the Treatment of the Whole Person
Introduction
In clinical practice, it is common to see complex patients with a combination of impairments in multiple systems including the musculoskeletal, urogynecological, respiratory and sensory/equilibrium. A thorough evaluation often reveals many movement habits, past injuries, thoughts/beliefs, and emotional states that have collectively led to changes in strategies for posture, movement, continence and organ support. Should the location of pain, or the primary region of impairment, direct the location and focus of treatment? In other words, does pelvic girdle pain, with or without incontinence and/or prolapse mean that the pelvis requires treatment? Can approaches that classify pain states and behavior always predict treatment outcomes? Butler notes that,
“The word“division”can be instant trouble because these mechanisms all occur in a continuum. All pain states probably involve all mechanisms, however in some, a dominance of one mechanism may become obvious. Pain mechanisms are not diseases or specific injuries. They simply represent a process or biological state.”(Butler 2000).
There is little scientific evidence to guide clinicians for these complex, yet common, patients. Jull(2012)notes that clinical reasoning remains the recommended approach for determining best treatment for the individual patient. Given the same painful impairment, no two individuals will have exactly the same experience and behavior because how they manifest their pain or illness is shaped in part by who they are(Jones & Rivett 2004)what they think and how they feel. There are sensorial, cognitive and emotional dimensions that are individual to every experience. The Integrated Systems Model for Disability & Pain(ISM)is an evidence-based clinical reasoning approach that considers all three dimensions of the patient’s experience to facilitate decision-making and treatment planning.
The Integrated Systems Model for Disability & Pain
The Integrated Systems Model for Disability and Pain(ISM)(Lee L-J and Lee D 2011)is not a protocol nor a classification but rather a framework to help clinicians organize knowledge and develop clinical reasoning to facilitate wise decisions for treatment. The Clinical Puzzle(figure right)is a graphic that conceptualizes this model and is used as a reflection tool for the development of clinical reasoning and ultimately clinical expertise. The patient’s goals and meaningful complaints are noted in the center of the Clinical Puzzle and from their story a meaningful task is identified.
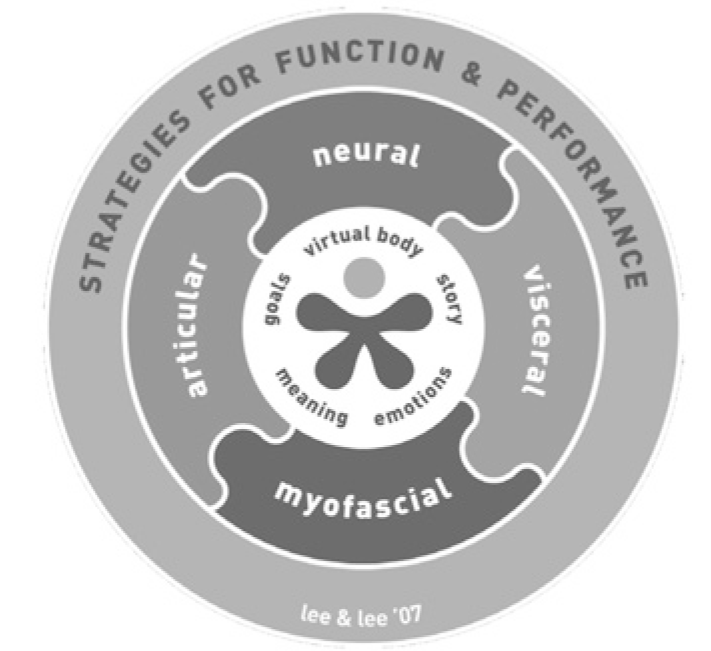
Two to three screening tasks that pertain to their meaningful task are listed in the outer circle(strategies for function and performance)of the Clinical Puzzle and key results from strategy analysis of each task are listed. For example, if the patient’s primary complaint is pelvic girdle pain(PGP)aggravated by sitting, then three meaningful screening tasks that relate to sitting would be:
1. standing posture
2. squat
3. sitting posture.
Each of these tasks would then be assessed to determine if the strategy chosen was optimal for both function and performance of the task. An optimal strategy produces appropriate alignment, biomechanics and control for the whole body/person. Optimal strategies allow the body to distribute and share loads effectively and safely.
A key feature of The Integrated Systems Model approach is Finding the Primary Driver(the best place to focus treatment). In short, this involves understanding the relationships between、and within, multiple regions of the body and how impairments in one region can impact the other. Specific tests are used to determine sites of non-optimal alignment, biomechanics and control(defined as failed load transfer).
Subsequently, the timing of failed load transfer(which site fails first, second, third etc.), as well as the impact of manually correcting one site on another, is noted. Clinical reasoning of the various results determines the site of the primary driver, or the primary region of the body, that if corrected will have a significant impact on the function of the whole body/person.
In the squat task below, three sites of failed load transfer were noted;the right sacroiliac joint gave way(i.e. the right innominate anteriorly rotated relative to the sacrum), the right hip translated anterior relative to the innominate(failed to remain centered in the hip joint)and the 4th thoracic ring translated to the left/rotated to the right. Where should treatment begin, the pelvis, hip or thorax? In other words, which region of the body is the primary driver?
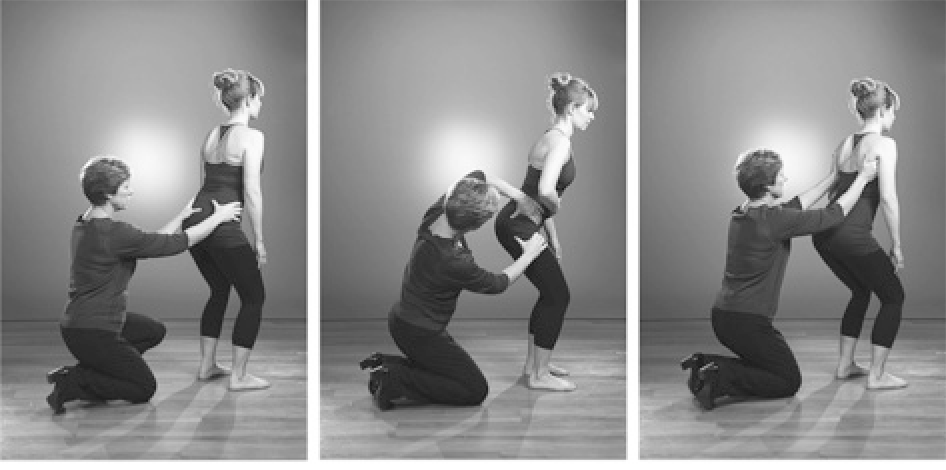
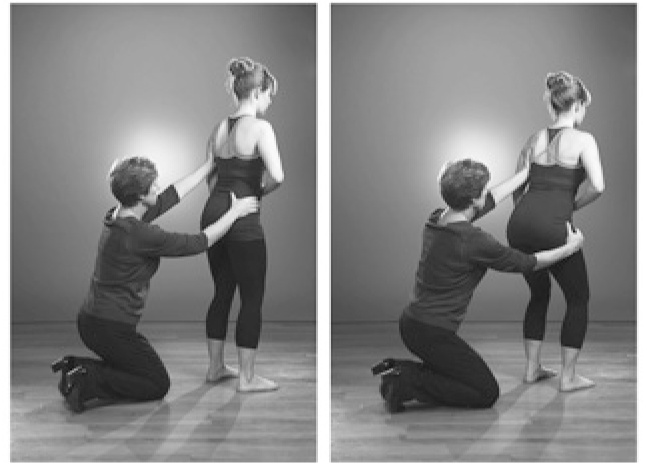
Timing of failed load transfer:The 4th thoracic ring translated to the left before the right sacroiliac joint gave way(figure above left)and before the right femoral head translated anteriorly(figure above right), this suggests that the 4th thoracic ring is the primary driver for this task.
Impact of corrections:This hypothesis was confirmed when manually correcting the 4th thoracic ring(correcting its alignment, biomechanics and control for this task)produced optimal function of the right SIJ and hip.
Further tests directed to the 4th thoracic ring then determined the underlying system impairment(e.g. articular, neural, myofascial, visceral)causing the non-optimal alignment, biomechanics and/or control for this squat task. Once the impaired system is determined, specific techniques and training for release, alignment, control and integration into movement(including strength and conditioning)can be implemented to improve the function of the primary driver(4th thoracic ring in this case)and thus impact the function of the whole body/person.
This keynote presentation will go deeper into the various aspects of The Integrated Systems Model for Disability & Pain(Lee & Lee)through short clinical case reports. The principles for treatment will also be outlined. For more information The 4th Edition of The Pelvic Girdle(Lee D 2011)is now translated into Japanese and is a valuable resource for more information.
References
Jull G 2012 Management of cervical spine disorders:where to now? IFOMPT Quebec City, Canada
Butler D S 2000 The sensitive nervous system. NOI Group Publications, Adelaide, Australia
Jones M A, Rivett D 2004 Introduction to clinical reasoning. In:Jones M A, Rivett D A(eds)Clinical reasoning for manual therapists. Elsevier, Edinburgh p 3
Lee D 2011 The Pelvic Girdle, An Integration of Clinical Expertise and Research, Churchill Livingstone, Elsevier, Edinburgh
Lee L-J, Lee D 2011 Clinical Practice-The Reality for Clinicians. Chapter 7 in:2011, The Pelvic Girdle, 4th edn. Elsevier, Edinburgh
In clinical practice, it is common to see complex patients with a combination of impairments in multiple systems including the musculoskeletal, urogynecological, respiratory and sensory/equilibrium. A thorough evaluation often reveals many movement habits, past injuries, thoughts/beliefs, and emotional states that have collectively led to changes in strategies for posture, movement, continence and organ support. Should the location of pain, or the primary region of impairment, direct the location and focus of treatment? In other words, does pelvic girdle pain, with or without incontinence and/or prolapse mean that the pelvis requires treatment? Can approaches that classify pain states and behavior always predict treatment outcomes? Butler notes that,
“The word“division”can be instant trouble because these mechanisms all occur in a continuum. All pain states probably involve all mechanisms, however in some, a dominance of one mechanism may become obvious. Pain mechanisms are not diseases or specific injuries. They simply represent a process or biological state.”(Butler 2000).
There is little scientific evidence to guide clinicians for these complex, yet common, patients. Jull(2012)notes that clinical reasoning remains the recommended approach for determining best treatment for the individual patient. Given the same painful impairment, no two individuals will have exactly the same experience and behavior because how they manifest their pain or illness is shaped in part by who they are(Jones & Rivett 2004)what they think and how they feel. There are sensorial, cognitive and emotional dimensions that are individual to every experience. The Integrated Systems Model for Disability & Pain(ISM)is an evidence-based clinical reasoning approach that considers all three dimensions of the patient’s experience to facilitate decision-making and treatment planning.
The Integrated Systems Model for Disability & Pain
The Integrated Systems Model for Disability and Pain(ISM)(Lee L-J and Lee D 2011)is not a protocol nor a classification but rather a framework to help clinicians organize knowledge and develop clinical reasoning to facilitate wise decisions for treatment. The Clinical Puzzle(figure right)is a graphic that conceptualizes this model and is used as a reflection tool for the development of clinical reasoning and ultimately clinical expertise. The patient’s goals and meaningful complaints are noted in the center of the Clinical Puzzle and from their story a meaningful task is identified.
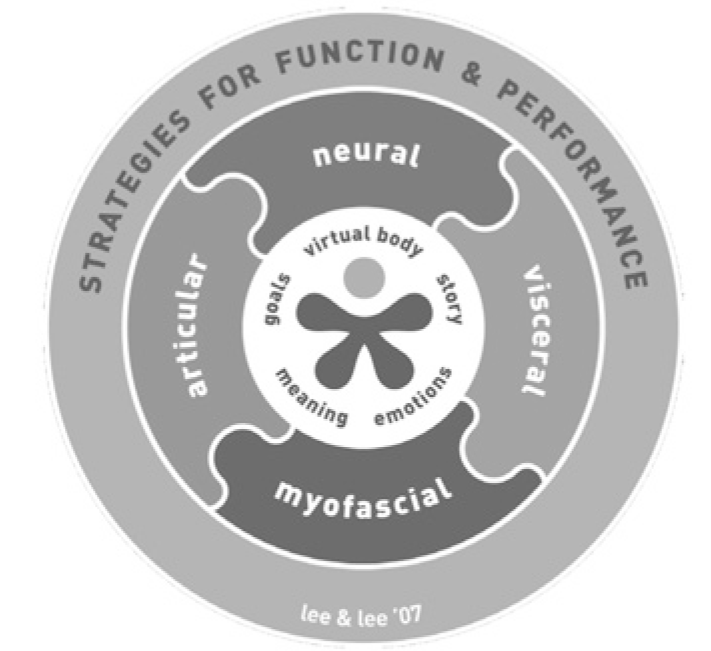
Two to three screening tasks that pertain to their meaningful task are listed in the outer circle(strategies for function and performance)of the Clinical Puzzle and key results from strategy analysis of each task are listed. For example, if the patient’s primary complaint is pelvic girdle pain(PGP)aggravated by sitting, then three meaningful screening tasks that relate to sitting would be:
1. standing posture
2. squat
3. sitting posture.
Each of these tasks would then be assessed to determine if the strategy chosen was optimal for both function and performance of the task. An optimal strategy produces appropriate alignment, biomechanics and control for the whole body/person. Optimal strategies allow the body to distribute and share loads effectively and safely.
A key feature of The Integrated Systems Model approach is Finding the Primary Driver(the best place to focus treatment). In short, this involves understanding the relationships between、and within, multiple regions of the body and how impairments in one region can impact the other. Specific tests are used to determine sites of non-optimal alignment, biomechanics and control(defined as failed load transfer).
Subsequently, the timing of failed load transfer(which site fails first, second, third etc.), as well as the impact of manually correcting one site on another, is noted. Clinical reasoning of the various results determines the site of the primary driver, or the primary region of the body, that if corrected will have a significant impact on the function of the whole body/person.
In the squat task below, three sites of failed load transfer were noted;the right sacroiliac joint gave way(i.e. the right innominate anteriorly rotated relative to the sacrum), the right hip translated anterior relative to the innominate(failed to remain centered in the hip joint)and the 4th thoracic ring translated to the left/rotated to the right. Where should treatment begin, the pelvis, hip or thorax? In other words, which region of the body is the primary driver?
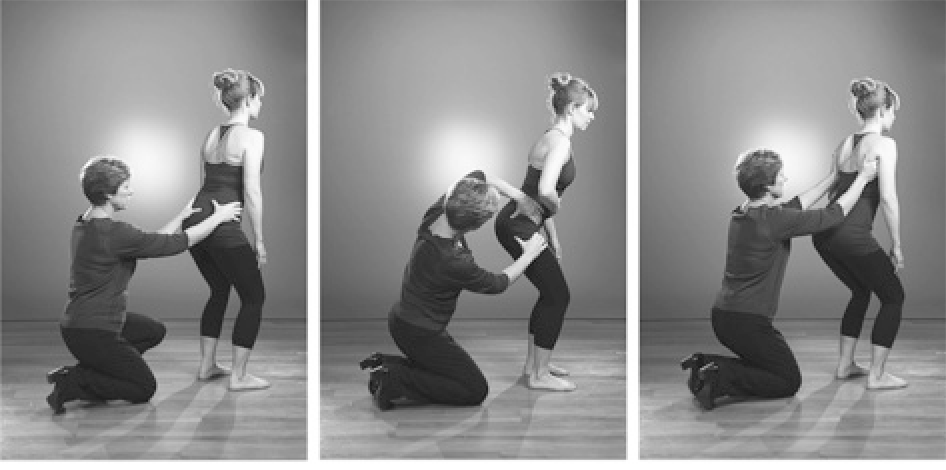
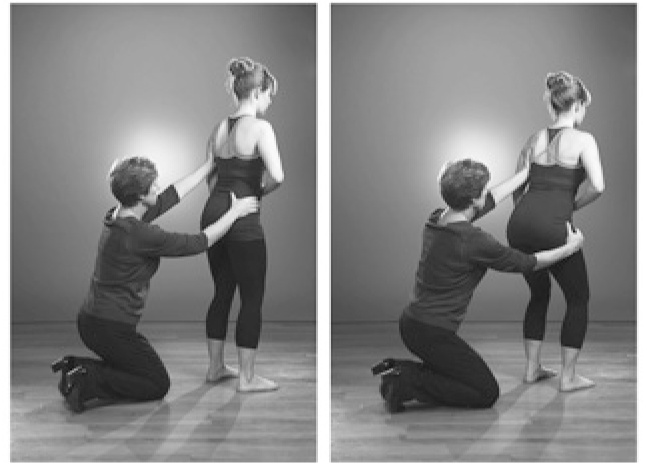
Timing of failed load transfer:The 4th thoracic ring translated to the left before the right sacroiliac joint gave way(figure above left)and before the right femoral head translated anteriorly(figure above right), this suggests that the 4th thoracic ring is the primary driver for this task.
Impact of corrections:This hypothesis was confirmed when manually correcting the 4th thoracic ring(correcting its alignment, biomechanics and control for this task)produced optimal function of the right SIJ and hip.
Further tests directed to the 4th thoracic ring then determined the underlying system impairment(e.g. articular, neural, myofascial, visceral)causing the non-optimal alignment, biomechanics and/or control for this squat task. Once the impaired system is determined, specific techniques and training for release, alignment, control and integration into movement(including strength and conditioning)can be implemented to improve the function of the primary driver(4th thoracic ring in this case)and thus impact the function of the whole body/person.
This keynote presentation will go deeper into the various aspects of The Integrated Systems Model for Disability & Pain(Lee & Lee)through short clinical case reports. The principles for treatment will also be outlined. For more information The 4th Edition of The Pelvic Girdle(Lee D 2011)is now translated into Japanese and is a valuable resource for more information.
References
Jull G 2012 Management of cervical spine disorders:where to now? IFOMPT Quebec City, Canada
Butler D S 2000 The sensitive nervous system. NOI Group Publications, Adelaide, Australia
Jones M A, Rivett D 2004 Introduction to clinical reasoning. In:Jones M A, Rivett D A(eds)Clinical reasoning for manual therapists. Elsevier, Edinburgh p 3
Lee D 2011 The Pelvic Girdle, An Integration of Clinical Expertise and Research, Churchill Livingstone, Elsevier, Edinburgh
Lee L-J, Lee D 2011 Clinical Practice-The Reality for Clinicians. Chapter 7 in:2011, The Pelvic Girdle, 4th edn. Elsevier, Edinburgh
